To your surprise, after your esophagogastroduodenoscopy (EGD), your doctor tells you that you likely have Barrett’s esophagus. Maybe you’ve heard of it on a public service announcement about acid reflux and esophageal cancer. Or maybe it’s a brand-new term to you.
Regardless, we have you covered. Let’s take a look at what Barrett’s esophagus is (and isn’t).
- It is NOT cancer.
Make sure you read that correctly. NOT cancer. Breathe a sigh of relief.
- It is a precancerous condition.
Studies have shown that in a small percentage of cases, less than 1%, Barrett’s esophagus can lead to esophageal cancer.
- It is most likely caused by acid reflux.
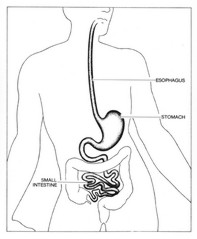
Your stomach is designed to withstand the acid it produces to help you digest your food. There is a valve at the top of the stomach, called the lower esophageal sphincter, to make sure stomach acid doesn’t harm any other part of your body. However, in some people, the lower esophageal sphincter doesn’t always close properly. This allows stomach acid to go up into your esophagus, which is the tube that connects your mouth to your stomach. When this occurs, it is called acid reflux or GERD (gastroesophageal reflux). Unlike the stomach, your esophagus is not designed to withstand stomach acid. After chronic exposure to the acid, the cells in the esophagus start to change. This is to protect them from the acid. This change can be seen with the naked eye during an EGD and must be confirmed with biopsies. The medical term for the change is Barrett’s esophagus.
- You may not know you have acid reflux.
Most people with acid reflux have symptoms which have prompted them to seek treatment. However, some people may not realize they’re having symptoms. Either their symptoms are so mild they don’t notice them, or the symptoms are occurring at night while they sleep. A small minority of people with Barrett’s esophagus do not have acid reflux at all.
- Treatment depends on the biopsies.
Your doctor will explain the best treatment for your Barrett’s once he receives the biopsy results. There are several different treatment options, depending on whether your Barrett’s has started to progress toward esophageal cancer.
- Your doctor will talk to you about ways to reduce acid reflux.
This can range from lifestyle changes, such as omitting certain foods from your diet, to elevating the head of your bed, to eating supper earlier in the day. Some of the foods which cause acid reflux most commonly include tomato-based products (such as spaghetti or pizza sauce), peppermint, caffeinated drinks, chocolate, and alcohol. It is best to allow 2-3 hours from the time of your last meal to bedtime to allow your food plenty of time to digest.
- Your doctor may recommend you start a medication for acid reflux.
He will discuss the risks and benefits of different medications and determine the best medication for you.
- Your doctor may recommend that you get regular EGDs to monitor the area.
Your doctor will take into account the severity of your Barrett’s and your overall health when making a recommendation about getting a repeat EGD to monitor the area. Monitoring helps your doctor know if the Barrett’s has progressed and whether treatment should change. It also helps catch a potential esophageal cancer early, which gives many more treatment options, as well as more favorable outcomes. But remember, less than 1% of cases of Barrett’s progress to esophageal cancer, so the odds are in your favor.
- If you smoke, your doctor will recommend that you quit.
You’re probably aware that smoking increases your risk for lung cancer. But it also increases your risk for a host of other cancers, including esophageal cancer. Now is the time to think hard about kicking the habit.
- Barrett’s esophagus is an area of active research.
As we learn more about Barrett’s esophagus, more treatment options will become available, and we’ll be able to better know the risk associated with the condition.
In the meantime, you’re in good hands!

Share This